Book Excerpt: Strategies for Enhancing Gut Balance
Photo Cred: BONDART PHOTOGRAPHY/Shutterstock
By Kellie Blake, RDN, LD, IFNCP
Bringing the gut microbiome back into balance requires a personalized, comprehensive plan. Since diet has the most overall impact on the composition of gut microbes, it’s important to choose a gut-friendly meal pattern and address your patient’s ability to digest and absorb nutrients. In addition, focusing on lifestyle strategies to target sleep, physical activity, and stress will be vital for achieving and maintaining gut microbiome balance.
Dietary Patterns
While specific foods and nutrients do significantly impact the gut microbiome, the dietary pattern overall is responsible for long-term gut microbiome health and the prevention of chronic inflammatory diseases (CIDs). The Western diet negatively impacts the gut microbiota, but there are several diets that have been found to support a healthy gut microbiome and thus decrease CID risk.
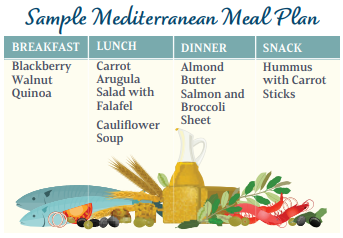
Mediterranean Diet
The Mediterranean diet has been studied extensively and is characterized by daily intake of unprocessed or minimally processed whole grains, cereals, legumes, seasonal fresh fruits and vegetables, nuts, seeds, and extra-virgin olive oil. In addition, there is low to moderate consumption of poultry, seafood, unprocessed or minimally processed cheese and yogurt, and wine with very low consumption of red and processed meats.
The Mediterranean diet is often recommended as a therapeutic diet for many CIDs, partially related to its ability to increase microbial diversity, (for example, higher levels of Bacteroidetes, Lactobacilli, Bifidobacteria, Faecalibacterium, Oscillospira, Rosburia, Ruminococci, and Clostridium cluster XiVa and lower levels of Firmicutes and Proteobacteria), SCFAs, and gut homeostasis, and ability to decrease gut dysbiosis, opportunistic pathobionts, and leaky gut. These effects on the gut microbiome are responsible for less oxidative stress and inflammation, improved immune function, and increased insulin sensitivity.
The Mediterranean diet is ideal for healthy patients wanting to prevent chronic disease development and for patients with chronic diseases who may not yet be ready to commit to a full elimination – type diet. I also use the Mediterranean diet as a base and then modify for patients with food sensitivities.
The Mediterranean diet can be considered an important dietary pattern for the prevention and treatment of metabolic syndrome, obesity, type 2 diabetes, CVD, bowel diseases, various cancers, and neurodegenerative disorders.
In addition, the Mediterranean diet has been proposed as one option for reducing frailty and ageing. In the NU-AGE dietary intervention project published in the journal Gut, a 12-month customized Mediterranean diet was found to modulate the gut microbiome in such a way as to reduce frailty and inflammation, but also enhance cognitive function of the participants.
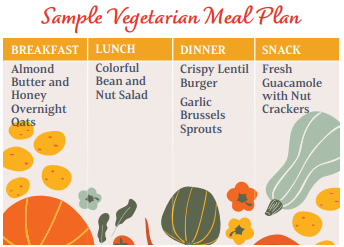
Vegan and Vegetarian Diet
Vegan and vegetarian diets have long been promoted as healthy dietary patterns overall and have been found to reduce the risk of CIDs and to also increase longevity. Vegan diets eliminate all animal products, while vegetarian diets may still allow eggs, fish, and dairy products. The influence of a plant-based diet on the gut microbiome is no doubt a significant part of the health-promoting effects of both these eating styles. Those following a vegan or vegetarian meal plan typically have a more diverse and stable gut microbiome when compared to meat eaters. Specifically, vegans and vegetarians have higher levels of Bacteroidetes, Ruminococcus, E. rectale, and Rosburia with lower levels of Clostridium and Enterococcus. Their higher intakes of polyphenols, which are found in plant foods, also increase levels of anti-inflammatory Bifidobacterium and Lactobacillus. In addition, the higher fiber intake in a vegan or vegetarian diet increases the production of SCFAs.
While a well-planned vegan or vegetarian diet can provide powerful health benefits, if foods high in sugar, inflammatory oils, and refined, highly processed foods are consumed as part of the dietary pattern, the positive benefits will be negated. Many of the plant-based substitutes available today contain inflammatory ingredients, which can contribute to dysbiosis and leaky gut.
I encourage all my patients to choose a plant-centric eating style. Vegan and vegetarian diets are beneficial for patients hoping to enrich the gut microbiome and prevent or reverse chronic inflammatory diseases. However, they need to be well-planned and nutritional supplements will likely be necessary, especially with the vegan diet.
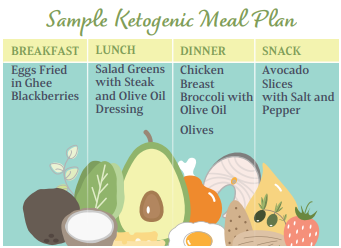
Ketogenic Diet
The ketogenic diet has become much more popular lately and there is research to support the use of this eating style in a variety of disease states. The ketogenic diet is typically very low in carbohydrates, approximately five to 10 percent of calories or less than 50 grams per day, and very high in fat. This eating style first became an important treatment for childhood epilepsy and part of the benefit lies in the alteration of the gut microbiome.
As reported in Genes, one study compared the changes to the microbiomes of 14 epileptic infants and 30 healthy infants after a ketogenic diet. In those with epilepsy, the gut microbiome was imbalanced with higher levels of pathogenic bacteria before initiation of the ketogenic diet. After the ketogenic diet, pathogenic bacteria levels had decreased. In both patient groups, there was an increase in Bacteroidetes, which is important in the regulation of interleukins that are connected to seizures in those with epilepsy.
A systematic review published in Genes reports the ketogenic diet reduces bacterial diversity overall, but has been found in mice to increase Akkermansia muciniphila and Lactobacillus, which are SCFA-producers. Other changes from the ketogenic diet include reduced amounts of pro-inflammatory microbes.
While the ketogenic diet does significantly decrease the amount of carbohydrate consumed, this does not have to lead to negative gut microbiome effects. A well-planned ketogenic diet, high in good-quality polyunsaturated fats can maintain normal gut function. In addition, supplementation with pre- and probiotics can be helpful in preventing gut microbiome changes on the ketogenic meal plan.
Combination diets are also an alternative to the strict ketogenic diet. One such example is the Modified Mediterranean Ketogenic Diet (MMKD), which follows ketogenic diet principles, but allows for higher intakes of fruits and vegetables. One intervention reported in EBioMedicine found the MMKD favorably modulated the gut microbiome in those with mild cognitive impairment to reduce cerebrospinal fluid markers of Alzheimer’s disease (AD).
I personally do not use the ketogenic diet in my practice, but it has been shown to be an effective option for patients with type 2 diabetes, neurodegenerative disorders, cancer, autism spectrum disorder, obesity, and epilepsy.
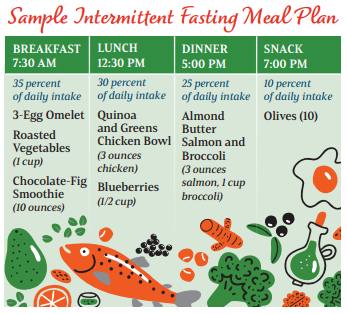
Fasting
The process of digesting and absorbing food is taxing on the body and allowing the body to rest from digestion can provide powerful health benefits. While calorie restriction has been shown to prevent and aid in the reversal of many health conditions, it is difficult to maintain, and long-term adherence is poor. Intermittent fasting, on the other hand, provides the same benefits of calorie restriction without the negative side effects.
Intermittent fasting improves insulin sensitivity, dyslipidemia, and inflammation, but also reduces visceral fat, improves mitochondrial function, and increases muscle mass. As reported in the journal Obesity, all forms of fasting allow the body to flip the metabolic switch to move from using glucose to fatty acids derived from ketones for energy. Another mechanism by which fasting improves health is via modulation of the gut microbiome. In fact, the Fasting Mimicking Diet (FMD) has been shown to stimulate protective gut microbiota in rat models. Additionally, according to a study published in the journal Cell Reports, after rats with inflammatory bowel disease (IBD) had gone through four cycles of the FMD, there was a three-fold increase in Lactobacillaceae, which functions to regulate T-cell activity and has been shown in experimental models to reduce the severity of IBD symptoms. In addition, Bifidobacteriaceae, which has reduced colitis symptoms in experimental models was enriched.
Fasting protocols should be tailored to the individual, but a daily 12-hour overnight fast is generally safe for most people and may provide some of its benefits via alterations to the gut microbiome. Since the gut microbiome operates on a circadian rhythm and is less diverse in the evening hours, I typically recommend my patients consume most of their daily food intake early in the day with breakfast and lunch and taper off in the evening. This may not always be possible for busy families but can provide powerful results.
Editor’s note: This article is an excerpt from the e-book Nutrition Foundations for the Gut Microbiome. Click here to read more.

















