Timing is everything part 1: The complexity and clinical consequences of circadian dyssynchrony
By Integrative Practitioner Staff
by Lena D. Edwards, MD, ABOIM, ABAARM, FAARM, FICT
The daily rotational cycles of the earth result in 24-hour cycles of alternating light and darkness. This rhythm affects the sustainability of life on this planet because it dictates global food availability, temperature, and light intensity. Human beings have evolutionarily adapted to this predictable cycle by creating internal clock systems, which synchronize all metabolic, cellular, and behavioral processes.
Extensive research has shown that the functional integrity of the human circadian clock system is a critical determinant of health, behavior, and disease development. In fact, even when other confounding comorbid factors are absent, circadian dyssynchrony can increase an individual’s risk of developing a number of diseases including diabetes, hypertension, a variety of malignancies, and cardiovascular disease, to name a few. Healthcare providers can better counsel and treat their patients when they understand the pathophysiological mechanisms by which ‘being out of rhythm’ can cause widespread physiologic disarray.
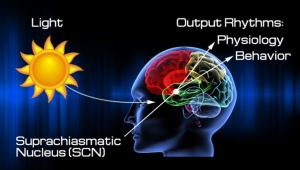
The central mediator of the circadian hierarchical clock system is the ‘master clock’ located in the suprachiasmatic nucleus (SCN) of the ventral hypothalamus. Remarkably, the 20,000 neurons located here are cell autonomous, individually capable of generating their own rhythmic oscillations. However, for optimal central clock function to occur, the SCN relies on a collaborative network comprised of a community of all individual, cell autonomous neurons. The innate function of the human circadian clock system is a genetically influenced; however its functional integrity is mediated by an intricate interplay of exogenous cues, endogenous hormonal mediators, and numerous molecular factors. Many types of exogenous cues, including light exposure (most “potent”), feeding times, physical activity, and sleep habits, can regulate SCN control of circadian rhythm.
There are three essential components of the human circadian clock system.
- The input pathways, which receive and relay exogenous cues to the brain
- A central circadian clock in the SCN, which maintains the circadian rhythm (“master clock”)
- Peripheral clocks within individual organs, which control the physiologic, behavioral, and metabolic end responses
Yes, you read correctly: individual organs, including the liver, intestines, adrenal glands, pancreas, heart, and brain, possess their own tissue-specific peripheral clock systems.
Unlike the cell autonomous networks of the central clock, the cellular networks of peripheral clocks are not autonomous, and thus rely on consistent communication with the central clock to synchronize with each other, and with the SCN. Since the discovery a little over a decade ago, ongoing studies of peripheral clocks have shown that they are extremely influential in coordinating numerous aspects of organ function. In fact, peripheral clocks regulate such a wide range of metabolic processes— including lipid metabolism, glucose metabolism, oxidative phosphorylation, and detoxification pathways—that any dyssynchrony with each other, or with the central clock, can directly impact an individual’s thoughts and behaviors, as well as their overall health and predilection for disease development.
The ultimate downstream hormonal mediator of the SCN induced circadian rhythm is cortisol. Due to its global physiologic authority over all bodily functions, cortisol serves as the key time-keeping chemical messenger. Regulation of cortisol secretion mandates global physiological and cellular function, and also affects the ongoing functional integrity of the circadian rhythm itself. There are three main pathways through which SCN stimulation induces cortisol release and regulation:
- Activation of the HPA axis with subsequent ACTH dependent cortisol release
- Direct neural connection between the SCN and the adrenal gland via the autonomic nervous system (ANS)
- Direct photic stimulation of the adrenal glands via SCN-ANS pathway, through catecholamine induced splanchnic nerve stimulation
Studies indicate that the latter two pathways outlined above are actually more important in initiating and maintaining the circadian rhythm. Contrary to conventional thinking, the HPA axis-dependent pathways appear to be more influential in regulating the adrenal response to stressors than in maintaining circadian rhythm. This becomes extremely important when we are examining our patient’s salivary cortisol release patterns.
In part 2 of this series, I will discuss the role the adrenal glands play in maintaining normal circadian rhythmicity.
References
Brown SA, Azzi A. Peripheral circadian oscillators in mammals. Handb Exp Pharmacol. 2013;(217):45-66.
Buijs R, Salgado R, Sabath E, Escobar C. Peripheral circadian oscillators: time and food. Prog Mol Biol Transl Sci. 2013;119:83-103.
Challet E. Keeping circadian time with hormones. Diabetes Obes Metab. 2015 Sep;17 Suppl 1:76-83.
Chung S, Son GH, Kim K.Circadian rhythm of adrenal glucocorticoid: its regulation and clinical implications. Biochim Biophys Acta. 2011 May;1812(5):581-91.
Dickmeis T. Glucocorticoids and the circadian clock. J Endocrinol. 2009 Jan;200(1):3-22.
Hastings MH, Reddy AB, Maywood ES. A clockwork web: circadian timing in brain and periphery, in health and disease. Nat Rev Neurosci. 2003; 4: 649–661.
Johnston JD. Physiological links between circadian rhythms, metabolism and nutrition. Exp Physiol. 2014 Sep;99(9):1133-7.
Kalsbeek A, van der Spek R, Lei J, Endert E, Buijs RM, Fliers E. Circadian rhythms in the hypothalamo-pituitary-adrenal (HPA) axis. Mol Cell Endocrinol. 2012 Feb 5;349(1):20-9.
Ota T1, Fustin JM, Yamada H, Doi M, Okamura H. Circadian clock signals in the adrenal cortex. Mol Cell Endocrinol. 2012 Feb 5;349(1):30-7.
Paschos GK. Circadian clocks, feeding time, and metabolic homeostasis. Front Pharmacol. 2015 May 27;6:112.
Ramkisoensing A, Meijer JH. Synchronization of Biological Clock Neurons by Light and Peripheral Feedback Systems Promotes Circadian Rhythms and Health. Front Neurol. 2015 Jun 5;6:128.