Sarcopenic Diabetes: The Little-Known Complication Carrying High Risks
By Irene Yeh
In 2025, the Diabetes Atlas from the International Diabetes Foundation announced that 590 million people worldwide were diagnosed with diabetes, with about 40% believed to be underdiagnosed. Type 2 diabetes accounts for about 90% of diabetes cases on a worldwide level, and there are several detrimental side effects, such as insulin resistance, vision problems, and diabetic neuropathy. However, one little-known but common complication among patients is the progressive loss of muscle mass and strength. Known as sarcopenic diabetes, this condition affects about 1 in 4 people with type 2 diabetes and carries a higher risk of frailty, disability, longer hospitalization, and increased risk of death, as well as heart failure and chronic kidney disease. Yet it is seldom talked about.
The European Society for Clinical Nutrition and Metabolism (ESPEN) and the Diabetes Nutrition Study Group (DNSG) published a paper reviewing clinical studies of diabetes and muscle loss correlations (Clinical Nutrition, DOI: 10.1016/j.clnu.2025.10.007). The purpose of the paper is to increase awareness, encourage research efforts, and improve detection of sarcopenic diabetes.
Factors Behind Sarcopenic Diabetes
Several factors are involved in the complex link between muscle loss and diabetes. These include the following:
- Lifestyle habits: An unhealthy diet and lack of exercise are major causes behind weight gain, excess body fat, and type 2 diabetes, as well as a driver behind poor blood sugar control for people with type 1 diabetes. High caloric foods, unhealthy fats, and sugary foods can directly damage muscle metabolism by increasing inflammation and stressing muscle cells. Not eating enough high-quality protein and being physically inactive can further weaken muscles.
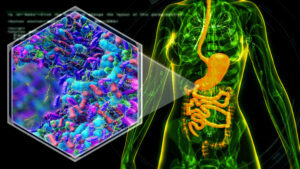
- Excess body fat: When the body cannot store extra fat, it leads to enlarged fat cells and reduced blood flow to tissues. This causes fat tissue to release inflammatory signals that disrupt normal metabolism. Fat also builds around organs, such as the liver and the muscles, which causes further metabolic damage.
- Inflammation and insulin resistance: An unhealthy lifestyle and excess body fat can result in ongoing inflammation throughout the body. This can lead to insulin resistance, which damages insulin-producing cells and increases blood sugar levels. Additionally, inflammation and insulin resistance disrupts how muscle proteins are built and broken down, resulting in reduced ability for muscles to repair themselves, stressed blood vessels, and poorer blood supply to muscle tissues, which further contributes to muscle loss.
- Hyperglycemia: When excess sugar attaches to muscle proteins, it forms advanced glycation end products (AGE), which promote muscle loss and dysfunction. Studies have shown that high blood sugar is linked to muscle loss, weaker muscles, and reduced strength, and these findings are confirmed to be present alongside other health problems. For example, people with heart failure and type 2 diabetes show damage to muscle cells, smaller muscle fibers, and poorer blood circulation to muscles. Research has also shown that hyperglycemia worsens overall protein loss in people with diabetes and kidney disease. Cancer patients with better blood sugar control have reduced muscle breakdown. Overall, sugar levels correlate with muscle loss and weakness, especially when combined with other diseases.
- Diabetic complications: Complications associated with diabetes and comorbidities (e.g., heart disease, kidney disease, and nerve damage) are linked to higher prevalence of sarcopenia. Nerve damage in particular can directly cause muscle atrophy by disrupting the connection between nerves and muscles and by reducing physical activity. Studies have shown that people with peripheral neuropathy often have lower muscle mass in affected areas. Evidence also shows that poor blood flow to the legs due to peripheral vascular disease is closely associated with impaired muscle metabolism and reduced muscle function.
- Anti-obesity and antidiabetic medications: Incretin-mimetic drugs (IMDs) have shown to help with improving blood sugar control, reducing body weight, and lowering heart and metabolic risks. Second-generation IMDs have also been approved for obesity treatment and have shown effectiveness for treating obesity and can lead to substantial weight loss. However, with large weight loss comes muscle loss. Typically, about one-quarter to one-third of the weight loss comes from lean tissue, including muscle. Naturally, this can result in sarcopenia.
Correlations Found
A large review of 20 studies with more than 54,000 participants reported that approximately 28% of people with type 2 diabetes had sarcopenia, which represents a 60% higher risk compared to people without diabetes. In the same analysis, 1,800 patients with diabetic-related complications had more than twice the risk of sarcopenia. Another analysis investigated sarcopenic obesity and found a similar prevalence of about 27% in the diabetes group and showed increased chances of complications and poor health outcomes. According to this analysis, patients with type 2 diabetes were confirmed for higher risk of sarcopenia due to reduced muscle strength. Across individual studies, the reported prevalence was between 5% to 50%, but poor blood sugar control was linked to higher risk of muscle loss.
The wide variation in reported rates likely reflects differences in age, sex, disease severity, and the population studied, as well as major differences in how sarcopenia was defined. Among the 20 studies reviewed, many inaccurately defined sarcopenia based only on low muscle mass, which is not consistent with current accepted definitions of sarcopenia and sarcopenic obesity that also includes low muscle function. Nonetheless, these findings support the fact that sarcopenia is a common but overlooked complication of diabetes.
Why Does This Matter?
Diabetes increases the risk of muscle loss, but muscle loss also increases the risk of developing diabetes and makes blood sugar levels harder to control, resulting in a harmful cycle. Sarcopenic diabetes can lead to frailty, disability, and loss of independence. It can also result in longer hospitalizations and increased mortality in older patients and people with diabetes treated outside a clinical setting. Furthermore, both diabetes and sarcopenia increase the risk of osteoporosis and bone fractures, culminating in osteosarcopenia, or bone and muscle loss occurring simultaneously.
ESPEN and DNSG are issuing a call to action to all stakeholders, including healthcare professionals, scientists, professional scientific societies, policymakers, the industry, and patients, to promote sarcopenic diabetes awareness, diagnosis, and treatment. Although evidence remains limited on how to best identify and treat sarcopenic diabetes, ESPEN and DNSG aim to offer practical, consensus-based guidance on how to prevent, diagnose, and manage sarcopenic diabetes using the available evidence for both diabetes and muscle loss, with or without obesity.
How to Approach Assessment, Diagnosis, and Treatment
The prevention, limitation, or treatment of sarcopenia should be a major clinical goal for patients with diabetes with the following conditions: symptoms of muscle loss and function, at-risk conditions of muscle loss and function (e.g., sedentary lifestyle, poor glycemic control, diabetic complications), and ongoing weight management programs including intensive lifestyle changes and medications such as IMDs.
Diagnosis has been elusive and difficult due to a lack of consensus from both research and clinical fields. There are established methods for sarcopenia in older adults, and the global leadership initiative on sarcopenia recently introduced an international-level consensus-based definition. In 2022, ESPEN and the European Association for the Study of Obesity created a consensus method for diagnosing sarcopenic obesity. This method was developed through the Sarcopenic Obesity Global Leadership Initiative (SOGLI), which also worked to spread awareness and guide research and clinical practice. SOGLI’s approach has been effective in identifying people with sarcopenic obesity and predicting who is at higher risk of poor health outcomes.
ESPEN and DNSG also envision collaborations to develop a diabetes-oriented strategy to optimize sarcopenic diabetes identification. Potentially, this would involve diabetes-specific parameters, such as directing glycemic control and managing diabetic complications. In addition, there should be nutritional assessments included, as well as functional status of patients with sarcopenic diabetes, specifically in the presence of complications and comorbidities.
Attention must also be given to type 1 diabetes, where complications can have a negative effect on muscle mass and function. With increasing rates of obesity among children and young adults, epidemiological shifts enhance the prevalence of previously described metabolic conditions with a negative impact on muscle loss and function in type 1 diabetes. As such, patients with type 1 diabetes must also be prioritized for obesity prevention, diabetes complications, and sarcopenia.
Managing Comorbidities and Other Conditions
For obesity patients with or without diabetes, weight loss can reduce both fat and muscle mass. Though fat loss is usually greater than muscle mass, that is not necessarily the case for older adults or those with chronic inflammatory or catabolic (destructive metabolism) conditions. And new weight loss drugs can further contribute to muscle loss. More research must be done to fully assess the effects of these drugs, particularly across different ages, levels of glycemic control, and presence of diabetes complications. The balance between fat loss and muscle loss requires careful monitoring.
Nutrition also plays a big role. In states of severe illness or prolonged underfeeding, accelerated muscle loss necessitates nutrition support with adequate calories and protein. Diabetes-specific nutrition plans may help with maintaining blood sugar while supporting muscle prevention. And, of course, physical activity also plays a role in managing glycemic levels and building and maintaining muscle mass.