Call your hospital’s on its integrative pain strategy: They are required to have one
 by John Weeks, Publisher/Editor of The Integrator Blog News and Reports Editor’s note: This analysis article is not edited and the authors are solely responsible for the content. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of Integrative Practitioner.
by John Weeks, Publisher/Editor of The Integrator Blog News and Reports Editor’s note: This analysis article is not edited and the authors are solely responsible for the content. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of Integrative Practitioner. The last two years have witnessed a snowstorm of governmental and quasi-governmental white papers arguing that non-pharmacologic, integrative medicine practices be considered first in pain care. The acronym soup of agencies and organizations includes FDA, CDC, NAM, ACP and the US Surgeon General.
The problem is that the recommendations have no teeth. The carrot of good science has only barely shifted the economically ingrained, reductive, pharma-focused practices. The powerful remedial action suggested by “non-pharma-first” and by the damage of the pharma model crisis lags.
Starting January 1, 2018, a useful stick has been paired with the carrot of sensible practice. Failure to offer a program of non-pharma pain services could result in a good thumping for a hospital or other delivery organization. The disciplinarian is the accrediting agency, the Joint Commission. The tool is the agency’s New and Revised Standards Related to Pain Assessment and Management.
The standards open potential for community activism. Call up your local hospital. Ask for the C-Suite of executive offices. Reference the Joint Commission’s Leadership Standards LD.04.03.13. Then ask these questions about steps they are required to take:
- Who is the hospital’s leader or leadership team responsible for pain management?
- What non-pharmacologic pain treatment modalities are they offering?
- What educational program do they have in place for staff and licensed independent practitioners on available services for consultation and referral of patients with complex needs?
 Let them know of community services and “licensed independent practitioners” in the community – you for instance! - who may not yet be included but could be useful for such complex and more simple patients with pain. Under the standard, the hospital is required to “either treat the patient’s pain or refer the patient for treatment.”
Let them know of community services and “licensed independent practitioners” in the community – you for instance! - who may not yet be included but could be useful for such complex and more simple patients with pain. Under the standard, the hospital is required to “either treat the patient’s pain or refer the patient for treatment.”
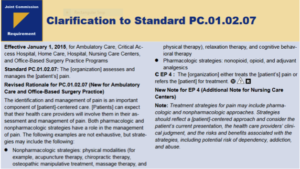
The Standard is not all that the integrative practice community wanted when it/we lobbied the Joint Commission last spring. It is clear the hospital must offer non-pharmacologic treatments. And notably, under “Elements of Performance PC.01.02.07,” they make a point of shuffling the language to list “non-pharmacologic” ahead of pharma. This alphabetical correction aligns them with a correct practice order.
Yet the language is less than optimal. An equivocating “may” pops up, like a snake in the grass: “Treatment strategies for pain may include nonpharmacologic, pharmacologic, or a combination of approaches.” What the heck is wrong, at this stage in the opioid crisis and advance of science on non-pharma practices, with upping the game with “shall”?
Nor does the standard that went into effect January 1, 2018 directly list the multiple integrative, non-pharma approaches that the Joint Commission has detailed elsewhere. For this, refer them to Clarification of Pain Management Standards PC.01.02.07. That “non-exhaustive” list is “physical modalities (for example, acupuncture therapy, chiropractic therapy, osteopathic manipulative treatment, massage therapy, and physical therapy), relaxation therapy, and cognitive behavioral therapy.”
 Yet one wonders why the Joint Commission chose to first put in teeth, then to file them down.
Yet one wonders why the Joint Commission chose to first put in teeth, then to file them down.
Is this some residue of the medical cold war regarding out-of-paradigm practices like acupuncture, mind-body and group-delivered services? Are they still kowtowing to conservative forces who believe patients are better dead than served by alt-med?
Consider the leadership the Joint Commission can yet provide in the crisis caused by over-reliance on pharma – for which they are partly to blame – if, in their new accreditation scoring they set a high bar for a hospital’s non-pharma programs then ruthlessly marked down slow-adopters. This language suggests that the agency will limit its service to public safety by choosing a non-activist role. Hospitals will continue to need additional external pressure to proactively serve up integrative pain care. Give yours a call.




















SHARE