 By Dr. Nancy Gahles, DC, CCH, RSHom(NA), OIM
By Dr. Nancy Gahles, DC, CCH, RSHom(NA), OIM Type 2 diabetes is knowingly amenable to diet and lifestyle changes. Reducing obesity, one of the comorbid conditions associated with Type 2 diabetes, has been shown to reduce risk.
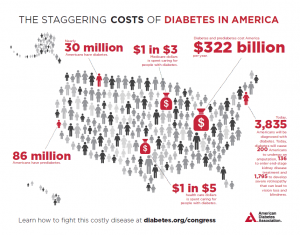
Diabetes represents one of the largest costs in our healthcare system. Healthcare professionals often mention lifestyle when discussing diabetes management. Generally, this refers to exercise, diet, and reducing stress.
The ubiquitous word
stress is often translated as a generalized sense of
angst or discomfort—irritation in everyday functions. Patients use the word “
stressed” on a daily basis to convey the etiology of their disease. A disease it is, and stressed they are, but how so?
The link between emotional stress and diabetes was recently the focus of a
study conducted at Rice University. (1) The research revealed a metabolic chain reaction that begins with low inhibition—that is, lack of attention control, an executive function of the brain. The subjects who had difficulty with attention control had increased vulnerability to more distraction in information, objects, thoughts, or activities leading to increased anxiety. The increased anxiety activated the metabolic pathway responsible for activation of the pro-inflammatory cytokines including interleukin- 6 (IL-6). IL-6 is a biomarker for stress that is associated with high glucose.
The
Rice University study lays the groundwork for investigation into the nature of anxiety, rumination on thoughts, their relationship to inflammation, and how stress manifests as a disease process unique to each individual.
An interesting lifestyle perspective from a homeopathic viewpoint is identifying the actual state of the person who is experiencing stress. Type 2 diabetes is a condition of starvation in the midst of plenty. Glucose piles up in the bloodstream and spills over into the urine and, yet, the individual cells are starved of glucose. More and more demand is placed upon the pancreas to secrete insulin to meet the needs of the increasing glucose but, alas, it is never enough. A maladaptation response goes into effect, and insulin resistance and inflammation ensue.
What is the emotional state of the person who is expressing this symptom? What are they anxious about? What is the exact stressor or stressors that challenge their ability to handle attention control, reasoning, and problem solving without the distractions and subsequent anxiety leading them down the primrose metabolic path to diabetes?
In my over 36 years of clinical practice, I have found one commonality in people with Type 2 diabetes: they suffer from some sort of grief. The nexus of the suffering in these people is loss. “Losing the sweetness in life” was the way in which one person described his descent into the feelings of loss. The stress of the loss has varied causations, among them are:
- Business failure
- Loss of position/job
- Loss of friendship
- Financial loss
- Emotional shocks, such as the loss of home or property
Prolonged and unresolved feelings cause chronic inflammation. According to the Rice University study, low inhibition begins the cycle. Individuals who are unable to gain mastery over their feelings are susceptible. In homeopathic literature, this is called diabetes of nervous origin.
When people suffering from diabetes are queried as to the causation of their emotional stress, they may name an actual event. When asked how they feel about it, a common response is, abandoned, deprived, or elements thereof. When asked how they have handled it, they are generally indifferent and appear apathetic or insensitive. In fact, one of the features of a useful homeopathic remedy in diabetes is its “insensitivity” to the action of insulin. The insensitivity of the person to the stressful event is a maladaptation—they suffer the ailments of grief, sorrow, and care, but cannot cry. They hold emotions inside, dwell on past disagreeable occurrences, and brood over unpleasant things.
Kyle Murdock, lead author of the Rice University study report, said that researchers have suspected a link between anxiety and poor health, including diabetes, for many years. “The literature shows individuals with poor inhibition are more likely to experience stressful thoughts and have a harder time breaking their attention away from them,” Murdock said. “This made me wonder if there’s a stress-induced pathway that could link inhibition with inflammation and the diseases we’re interested in, such as diabetes.”
The allostatic stress response network of nervous, endocrine, immune and metabolic pathways is one model to consider. Within the larger network is a hub that interacts with and adapts to any exogenous or endogenous stressor that disrupts homeostatic balance. Trauma, post-traumatic stress disorder, grief, loss, and the resultant rumination and inflammation appear to be the obvious culprits to stimulate the stress-induced pathways for the emergence of disease.
I concur with the suggestions of the researchers on several of the possible interventions, including mindfulness-based stress reduction (MBSR) and cognitive behavioral therapy (CBT). In my experience with diseases bearing emotional stress origin or imprint, the first intervention must be adaptive network nanomedicine. Dr. Iris Bell describes this intervention skillfully.
“As a low intensity stressor, remedy nanoparticles stimulate changes in the opposite direction to those of the higher intensity stressors that fostered the original development of disease,” she says. “The disease-related maladaptations prime the system, then the correct remedy in low dose elicits reversal of direction of the maladapted responses.” (2)
In my clinical experience, the disease-related maladaptations that prime the system cause the low inhibition. The selection of the appropriate nanomedicine reverses the maladaptation and restores flexibility in the brain’s executive functions. It is at this point that MBSR and CBT can work most efficiently to restore resilience and self-regulation.
The person is now capable of making conscious choices in their lifestyle to reduce their risk factors for diabetes and change the course of the disease.
RESOURCES:
- How inflammation bridges stress and diabetes. Psychoneuroendicrinology, June 7, 2016. Kyle Murdock. Rice University
- Extending the Adaptive Network Nanomedicine Model for Homeopathic Medicines: Nanostructures as Salient Cell Danger Signals for Adaptation. Iris R. Bell, Gary E. Schwartz, Joyce Frye, Barbara Sarter and Leanna J. Standish. Nanoscience & Technology:Open Access . June 14, 2015.
BIOGRAPHY
Dr. Nancy Gahles is an integrative and holistic doctor in family practice since 1980. She is owner of Health & Harmony Wellness Center and Spirit of Love~The Rockaway Sangha in Belle Harbor, NY. Dr. Gahles specializes in stress and its role in the cause of dis-ease. Her work developing the Triumvirate Technique© is informed by her experience as a chiropractor, a Certified Classical Homeopath, Certified Mindfulness Based Stress Reduction (MBSR) practitioner, Ordained Interfaith Minister and self-proclaimed Happiness Doctor. Dr. Gahles is a patient advocate and a political activist serving on the Board of Directors of the Integrative Health Policy Consortium (IHPC). She is President Emerita of the National Center for Homeopathy and serves on the Advisory Council of Homeopaths Without Borders and the Integrative Health Symposium.
She is a published author of
The Power of $elfCare: A Common Sense Guide to YOUR Wellness Solutionhttp://amzn.to/16G1hAB and TEDxTalk http://www.youtube.com/watch?v=l6bZBwl636s and ebook:
Health Investment Portfolios . Dr. Gahles is a member of the Association of Healthcare Journalists and Ethical Journalism.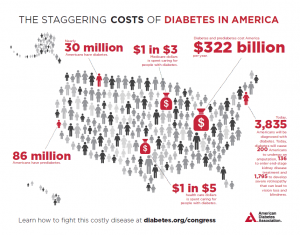 By Dr. Nancy Gahles, DC, CCH, RSHom(NA), OIM Type 2 diabetes is knowingly amenable to diet and lifestyle changes. Reducing obesity, one of the comorbid conditions associated with Type 2 diabetes, has been shown to reduce risk. Diabetes represents one of the largest costs in our healthcare system. Healthcare professionals often mention lifestyle when discussing diabetes management. Generally, this refers to exercise, diet, and reducing stress. The ubiquitous word stress is often translated as a generalized sense of angst or discomfort—irritation in everyday functions. Patients use the word “stressed” on a daily basis to convey the etiology of their disease. A disease it is, and stressed they are, but how so? The link between emotional stress and diabetes was recently the focus of a study conducted at Rice University. (1) The research revealed a metabolic chain reaction that begins with low inhibition—that is, lack of attention control, an executive function of the brain. The subjects who had difficulty with attention control had increased vulnerability to more distraction in information, objects, thoughts, or activities leading to increased anxiety. The increased anxiety activated the metabolic pathway responsible for activation of the pro-inflammatory cytokines including interleukin- 6 (IL-6). IL-6 is a biomarker for stress that is associated with high glucose. The Rice University study lays the groundwork for investigation into the nature of anxiety, rumination on thoughts, their relationship to inflammation, and how stress manifests as a disease process unique to each individual. An interesting lifestyle perspective from a homeopathic viewpoint is identifying the actual state of the person who is experiencing stress. Type 2 diabetes is a condition of starvation in the midst of plenty. Glucose piles up in the bloodstream and spills over into the urine and, yet, the individual cells are starved of glucose. More and more demand is placed upon the pancreas to secrete insulin to meet the needs of the increasing glucose but, alas, it is never enough. A maladaptation response goes into effect, and insulin resistance and inflammation ensue. What is the emotional state of the person who is expressing this symptom? What are they anxious about? What is the exact stressor or stressors that challenge their ability to handle attention control, reasoning, and problem solving without the distractions and subsequent anxiety leading them down the primrose metabolic path to diabetes? In my over 36 years of clinical practice, I have found one commonality in people with Type 2 diabetes: they suffer from some sort of grief. The nexus of the suffering in these people is loss. “Losing the sweetness in life” was the way in which one person described his descent into the feelings of loss. The stress of the loss has varied causations, among them are:
By Dr. Nancy Gahles, DC, CCH, RSHom(NA), OIM Type 2 diabetes is knowingly amenable to diet and lifestyle changes. Reducing obesity, one of the comorbid conditions associated with Type 2 diabetes, has been shown to reduce risk. Diabetes represents one of the largest costs in our healthcare system. Healthcare professionals often mention lifestyle when discussing diabetes management. Generally, this refers to exercise, diet, and reducing stress. The ubiquitous word stress is often translated as a generalized sense of angst or discomfort—irritation in everyday functions. Patients use the word “stressed” on a daily basis to convey the etiology of their disease. A disease it is, and stressed they are, but how so? The link between emotional stress and diabetes was recently the focus of a study conducted at Rice University. (1) The research revealed a metabolic chain reaction that begins with low inhibition—that is, lack of attention control, an executive function of the brain. The subjects who had difficulty with attention control had increased vulnerability to more distraction in information, objects, thoughts, or activities leading to increased anxiety. The increased anxiety activated the metabolic pathway responsible for activation of the pro-inflammatory cytokines including interleukin- 6 (IL-6). IL-6 is a biomarker for stress that is associated with high glucose. The Rice University study lays the groundwork for investigation into the nature of anxiety, rumination on thoughts, their relationship to inflammation, and how stress manifests as a disease process unique to each individual. An interesting lifestyle perspective from a homeopathic viewpoint is identifying the actual state of the person who is experiencing stress. Type 2 diabetes is a condition of starvation in the midst of plenty. Glucose piles up in the bloodstream and spills over into the urine and, yet, the individual cells are starved of glucose. More and more demand is placed upon the pancreas to secrete insulin to meet the needs of the increasing glucose but, alas, it is never enough. A maladaptation response goes into effect, and insulin resistance and inflammation ensue. What is the emotional state of the person who is expressing this symptom? What are they anxious about? What is the exact stressor or stressors that challenge their ability to handle attention control, reasoning, and problem solving without the distractions and subsequent anxiety leading them down the primrose metabolic path to diabetes? In my over 36 years of clinical practice, I have found one commonality in people with Type 2 diabetes: they suffer from some sort of grief. The nexus of the suffering in these people is loss. “Losing the sweetness in life” was the way in which one person described his descent into the feelings of loss. The stress of the loss has varied causations, among them are: 



















SHARE